Our billing service won’t nickel-and-dime your practice. You pay one predictable percentage of collections, see your reimbursements quickly, and have clear analytics to verify the results.
Dedicated billing experts stay current with the latest regulations to make sure claims meet all necessary standards, reducing the risk of compliance issues, so you have peace of mind.
Timely, accurate billing leads to quicker reimbursements and less confusion, which ultimately translates to more satisfied patients and a better care experience for them.
We’re a back-office partner for healthcare practices that want cleaner claims, faster decisions, and fewer surprises in their reimbursement cycle. With compliance-backed systems and a team that knows payers inside out, our job is to process claims to protect your revenue, claim by claim.
We’re here to help you do better financially by understanding your practice, building systems that fit your way of working and becoming a true partner. Our team works behind the scenes, handling claims, coding, denials, credentialing, and following up on AR so you can concentrate on helping patients.
Even the best in-house teams can encounter obstacles, from staff shortages to payer rule changes and backlogged AR. At Satti Technologies, we step in as a true extension of your hospital’s financial ecosystem, bringing structure, speed, and specialized oversight.
Preauthorization checks and insurance details are reviewed before care begins.
Each medically necessary service gets reviewed for coding and claim success.
HCPCS, CPT, and ICD-10 codes are applied based on patient treatment.
Before submitting, all claims are scrubbed against payer rules and audit flags.
Denials and underpayments are worked until every valid dollar owed is accounted for.
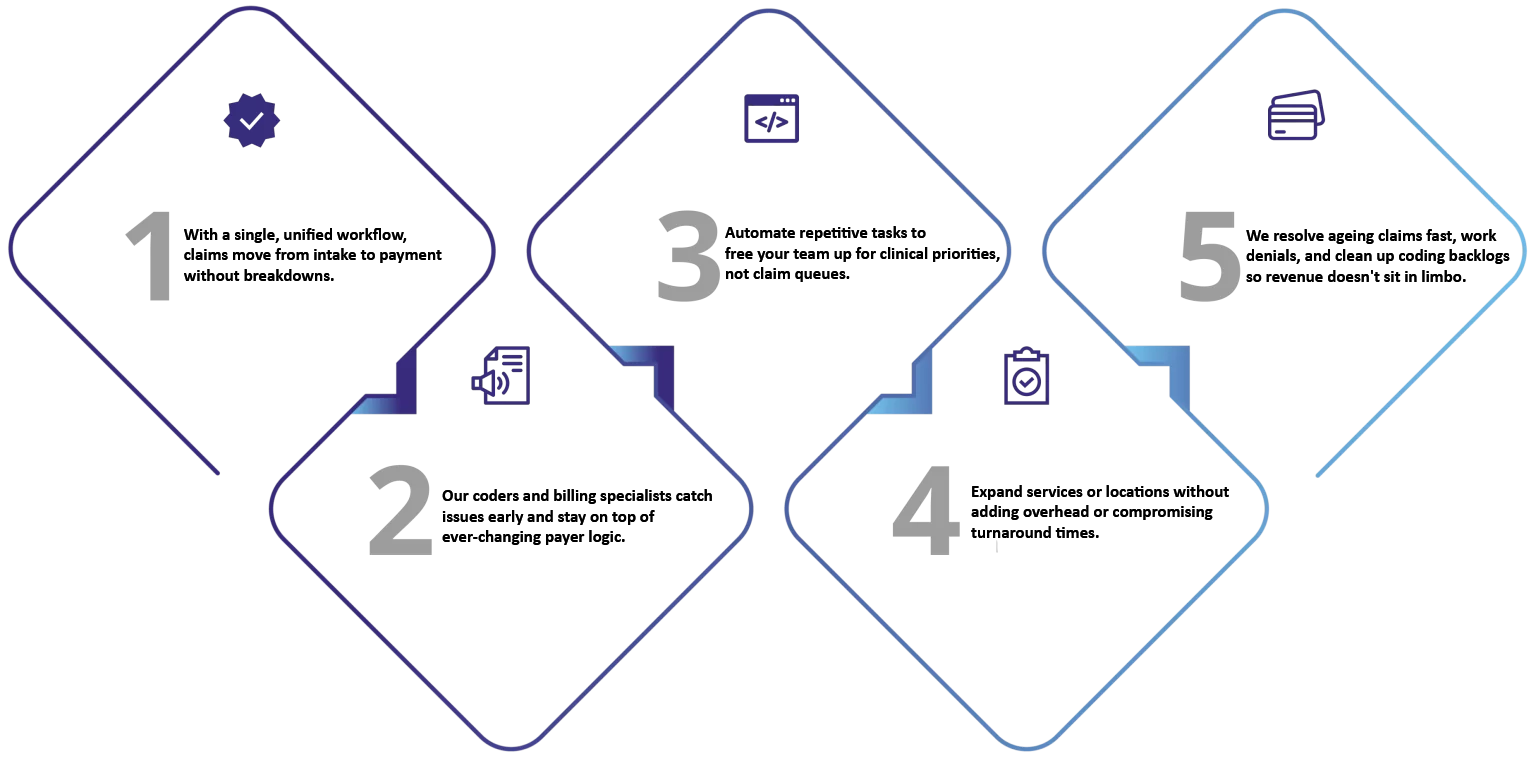
Our team helps healthcare practices build resilient revenue systems. With decades of on-ground experience in U.S. medical billing and compliance, we know how billing inefficiencies silently erode profitability. We step in as a strategic ally to protect your collections, reduce administrative noise, and give your clinical teams room to focus. Here’s how we do it:
Most practices are leaving 20–30% of their revenue uncollected, not because of care delivery, but because of avoidable billing errors. We’ve seen it firsthand. At Satti Technologies, we step in where the system fails such as, fixing coding gaps, flagging errors before submission, and chasing down every dollar that’s owed.
Let’s start with a free billing checkup.